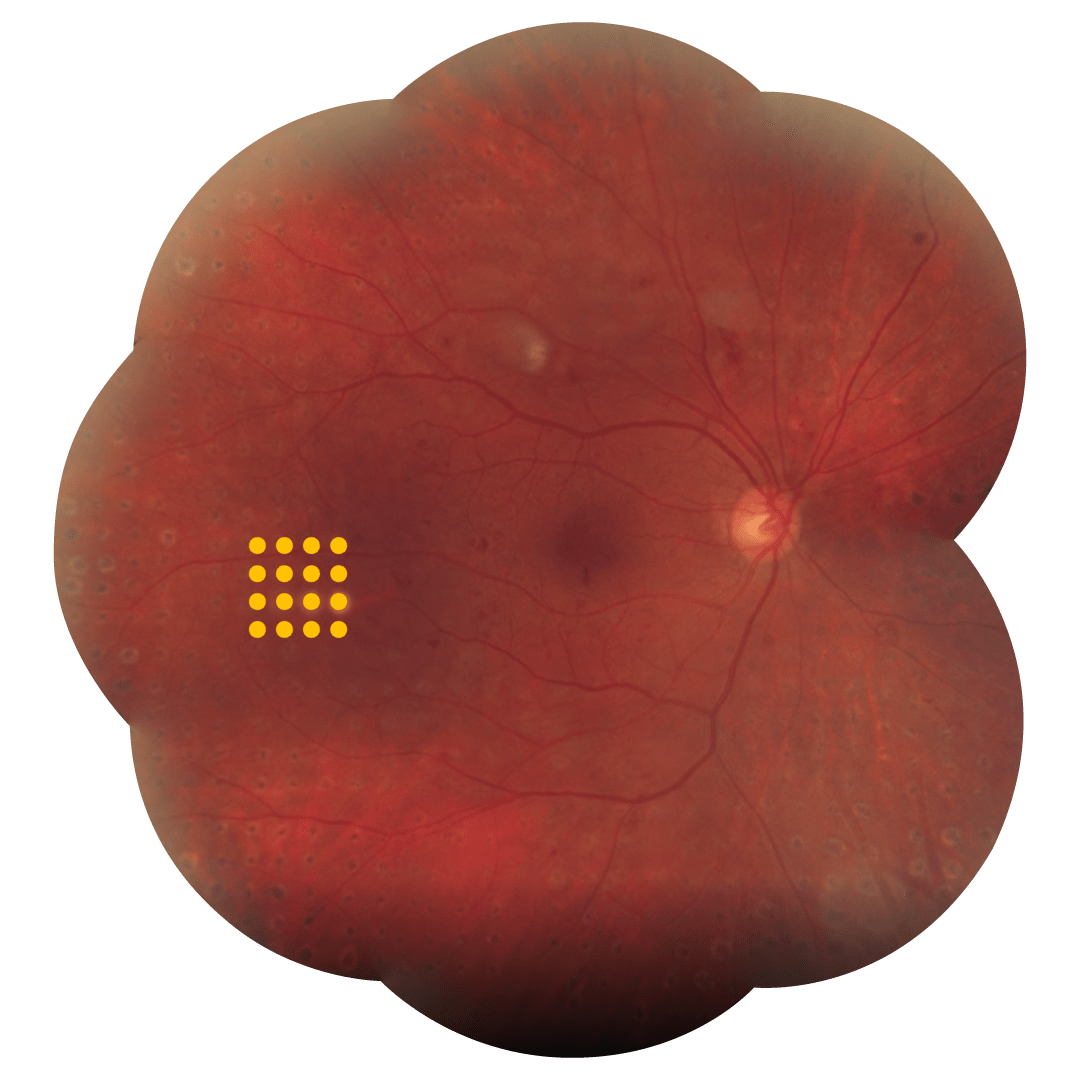
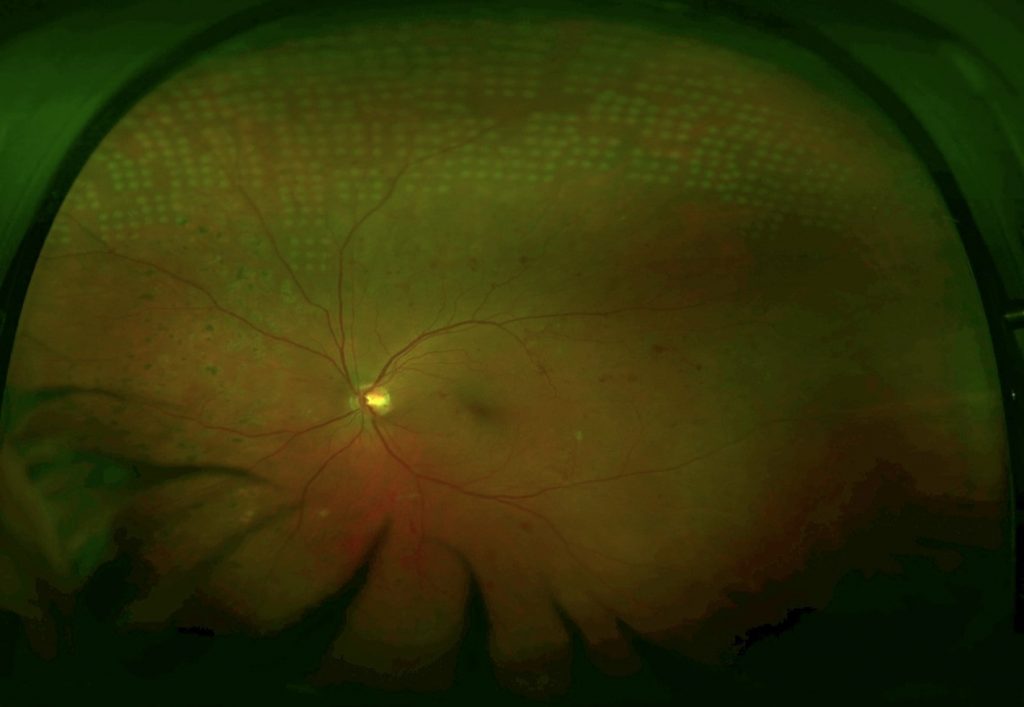
MultiSpot para tratamiento periférico
MultiSpot para tratamiento periférico
La fotocoagulación panretiniana (FPR) se ha mantenido como el estándar de atención para la retinopatía diabética (RD) avanzada desde finales de la década de 1970, cuando el Estudio de retinopatía diabética (DRS) y el Estudio de retinopatía diabética de tratamiento temprano (ETDRS)[1,2] informaron su beneficio en la prevención de la ceguera en las etapas proliferativas de la enfermedad.
La FPR convencional de un solo punto es intrínsecamente destructiva; sin embargo, en la última década se han introducido nuevas tecnologías que han dado lugar al desarrollo de una nueva generación de sistemas láser: los Láseres MultiSpot. Son capaces de producir pulsos de láser individuales más cortos en un orden de magnitud de 0.01s-0.02s. Al mismo tiempo, estos impulsos se dirigen en una secuencia rápida, uno tras otro, en los llamados patrones.
Pautas de tratamiento
La fotocoagulación láser MultiSpot es un método novedoso para suministrar energía láser a la retina.
Antes de comenzar el tratamiento con láser, es necesario valorar la energía láser necesaria para la producción de un punto láser (la duración del pulso es más corta).
Gracias a un solo punto, la energía láser se incrementa gradualmente hasta que se logra un punto láser gris.
A continuación, se puede seleccionar el patrón para el tratamiento.
Datos clinicos
Caracterizado por el uso de duraciones de pulso cortas (10-20ms), el modo de tratamiento MultiSpot ofrece muchas ventajas sobre la fotocoagulación convencional en tratamientos retinianos, como la fotocoagulación panretiniana (FPR):
- Menos difusión de calor a la retina y coroides, menos daño a la capa de fibras nerviosas de la retina1,2
- Tratamiento cómodo, mejor tolerado por los pacientes3
- Tratamiento extremadamente rápido (FPR completo en una sesión)4.
El modo de tratamiento MultiSpot se puede administrar a través de 4 patrones ajustables para una mejor adaptación al local de tratamiento: Cuadrados, círculos, triples arcos, un solo punto.
Anti-VEGF vs Laser for PDR, a changing treatment paradigm?




Médicos
Hablan deTerapia Láser
Multispot
Bibliografía
Objective: To systematically evaluate the effects of laser beam size, power, and pulse duration of 1 to 100 milliseconds on the characteristics of ophthalmoscopically visible retinal coagulation lesions.
Methods: A 532-nm Nd:YAG laser was used to irradiate 36 retinas in Dutch Belt rabbits with retinal beam sizes of 66, 132, and 330 mum. Lesions were clinically graded 1 minute after placement, their size measured by digital imaging, and their depth assessed histologically at different time points.
Results: Retinal lesion size increased linearly with laser power and logarithmically with pulse duration. The width of the therapeutic window, defined by the ratio of the threshold power for producing a rupture to that of a mild coagulation, decreased with decreasing pulse durations. For 132- and 330-mum retinal beam sizes, the therapeutic window declined from 3.9 to 3.0 and 5.4 to 3.7, respectively, as pulse duration decreased from 100 to 20 ms. At pulse durations of 1 millisecond, the therapeutic window decreased to unity, at which point rupture and a mild lesion were equally likely to occur.
Conclusions: At shorter pulse durations, the width and axial extent of the retinal lesions are smaller and less dependent on variations in laser power than at longer durations. The width of the therapeutic window, a measure of relative safety, increases with the beam size.
Clinical relevance: Pulse durations of approximately 20 milliseconds represent an optimal compromise between the favorable impact of speed, higher spatial localization, and reduced collateral damage on one hand, and sufficient width of the therapeutic window (> 3) on the other.
Purpose
To examine the effects of panretinal photocoagulation (PRP) using a pattern scanning laser (PASCAL) system on the retinal nerve fiber layer (RNFL) thickness in patients with diabetic retinopathy.
Methods
This retrospective study included 105 eyes with diabetic retinopathy, which consisted of three groups: the PASCAL group that underwent PRP with the PASCAL method (33 eyes), the conventional group that underwent conventional PRP treatment (34 eyes), and the control group that did not receive PRP (38 eyes). The peripapillary RNFL thickness was measured by optical coherence tomography before, six months, and one year after PRP to evaluate the changes in peripapillary RNFL.
Results
The RNFL thickness in the PASCAL group did not show a significant difference after six months (average 3.7 times, p = 0.15) or one year after the PRP (average 3.7 times, p = 0.086), whereas that in the conventional group decreased significantly after six months (average 3.4 times, p < 0.001) and one year after PRP (average 3.4 times, p < 0.001).
Conclusions
The results of this study suggest that the PASCAL system may protect against RNFL loss by using less energy than conventional PRP.
Purpose: We performed a study of laser panretinal photocoagulation in 20 patients with proliferative retinopathy. We compared short exposure, high-energy laser settings with conventional settings, using a 532 nm, frequency doubled, Neodymium-Yag laser and assessed the patients in terms of pain experienced and effectiveness of treatment.
Methods: Twenty patients having panretinal photocoagulation for the first time underwent random allocation to treatment of the superior and inferior hemi-retina. Treatment A used ‘conventional’ parameters: exposure time 0.1 s, power sufficient to produce a visible grey-white burns, spot size 300 microm. The other hemi- retina was treated with treatment B using exposure 0.02 s, 300 microm and sufficient power to have similar endpoint. All patients were asked to evaluate severity of pain on a visual analogue scale. (0=no pain, 10=most severe pain). All patients were masked as to the type of treatment and the order of carrying out the treatment on each patient was randomised. Patients underwent fundus photography and were followed up for 6-45 months.
Results: Seventeen patients had proliferative diabetic retinopathy, two had ischaemic central retinal vein occlusion and one had ocular ischaemic syndrome. The mean response to treatment A was 5.11, compared to 1.40 treatment B, on the visual analogue scale, which was statistically significant (P=0.001). All patients preferred treatment B. Further treatments, if required, were performed with treatment B parameters and long-term follow-up has shown no evidence of undertreatment.
Conclusions: Shortening exposure time of retinal laser is significantly less painful but equally effective as conventional parameters.
Objective: To investigate the effects of pattern scanning laser (Pascal; OptiMedica, Santa Clara, California) multispot panretinal photocoagulation given in a single-session (SS-PRP) vs single-spot multiple-session PRP (MS-PRP) on proliferative diabetic retinopathy (PDR).
Methods: Single-center, randomized clinical trial of 40 eyes. Proliferative diabetic retinopathy was treated with a 400-mum spot size in 1500 burns given either as Pascal in 20-millisecond SS-PRP or in 3 sessions (100-millisecond MS-PRP) during a 4-week period. Visual acuity, central subfield retinal thickness (CRT), and 24-2 Swedish interactive thresholding algorithm visual fields were recorded at baseline and 4 and 12 weeks.
Main outcome measures: Central subfield retinal thickness, mean deviation, and PDR grade at 12 weeks.
Results: There was a significant increase in mean CRT with MS-PRP (22 mum at 4 weeks, 95% CI, -32.25 to -10.75; 20 mum at 12 weeks, 95% CI, -28.75 to -10.82; P < .001) and no significant increase in the SS-PRP group. The mean deviation increased significantly in the SS-PRP group after 4 weeks (0.73 dB, P = .048), with no significant changes in either group at other points. A positive effect on PDR was observed in 74% of eyes in the SS-PRP group vs 53% in the MS-PRP group (P = .31). Mean treatment time for SS-PRP was 5.04 minutes (SD, 1.5 minutes) compared with 59.3 (SD, 12.7 minutes) in the MS-PRP group (P < .001).
Conclusions: There were no adverse outcomes (CRT, visual acuity, or visual field) from using multispot SS-PRP vs single-spot MS-PRP at 12 weeks postlaser, and treatment times were significantly shorter for multispot SS-PRP. Pascal SS-PRP was as effective as MS-PRP in the treatment of PDR.
Application to clinical practice: Twenty-millisecond Pascal SS-PRP may be safely and rapidly performed in 1500 burns with a similar efficacy to conventional MS-PRP. TRIAL IDENTIFIER: Research and Development Office PIN R00037, Central Manchester University Hospitals Foundation Trust.
