Terapia con Láser SubLiminal un tratamiento macular
Tratamiento macular
La terapia con láser SubLiminal se utiliza actualmente con mayor frecuencia en casos de enfermedades vasculares retinianas con edema macular, como el edema macular diabético (EMD) o la coriorretinopatía serosa central (CSC).
También se pueden considerar otras patologías maculares, como el edema macular secundario a oclusión de rama venosa retiniana (BRVO) o la vasculopatía coroidea polipoidea (PCV).
Pautas de tratamiento
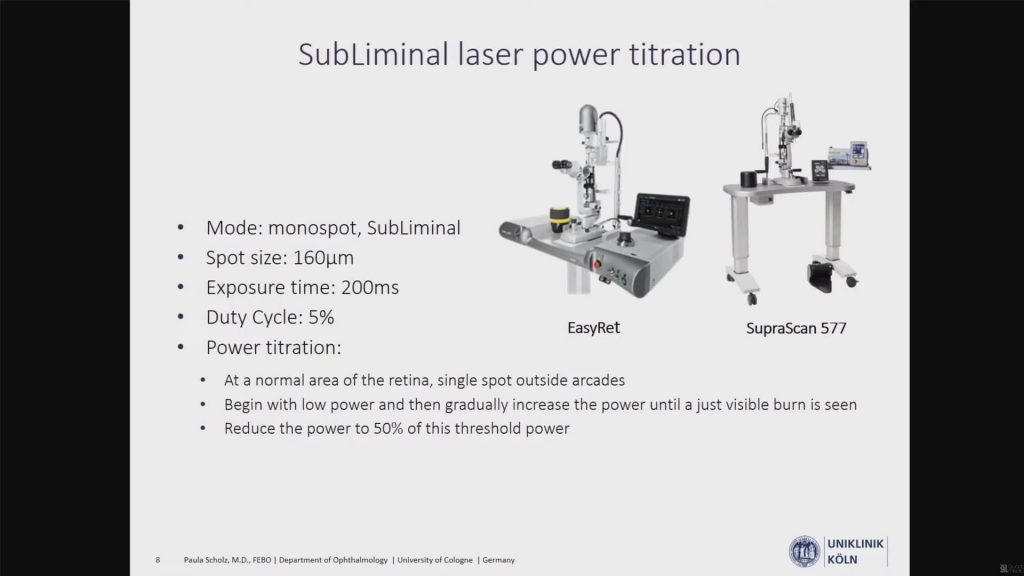
La terapia con láser SubLiminal es un método de suministro de energía láser a la retina que produce un efecto de bioestimulación al tiempo que minimiza el daño térmico permanente al tejido de la retina. El concepto implica administrar una «serie» de pulsos láser, cada pulso separado por el tiempo suficiente que permite la disipación del calor y reduce el daño permanente a la retina. A diferencia del tratamiento con láser macular convencional, no hay cicatrices visibles en el examen clínico, OCT o angiografía.
Consulte a continuación las pautas recomendadas para el tratamiento con láser SubLiminal preparadas por Victor Chong, MD (Reino Unido).
Basic Principles of MicroPulse Lasers

Datos clinicos
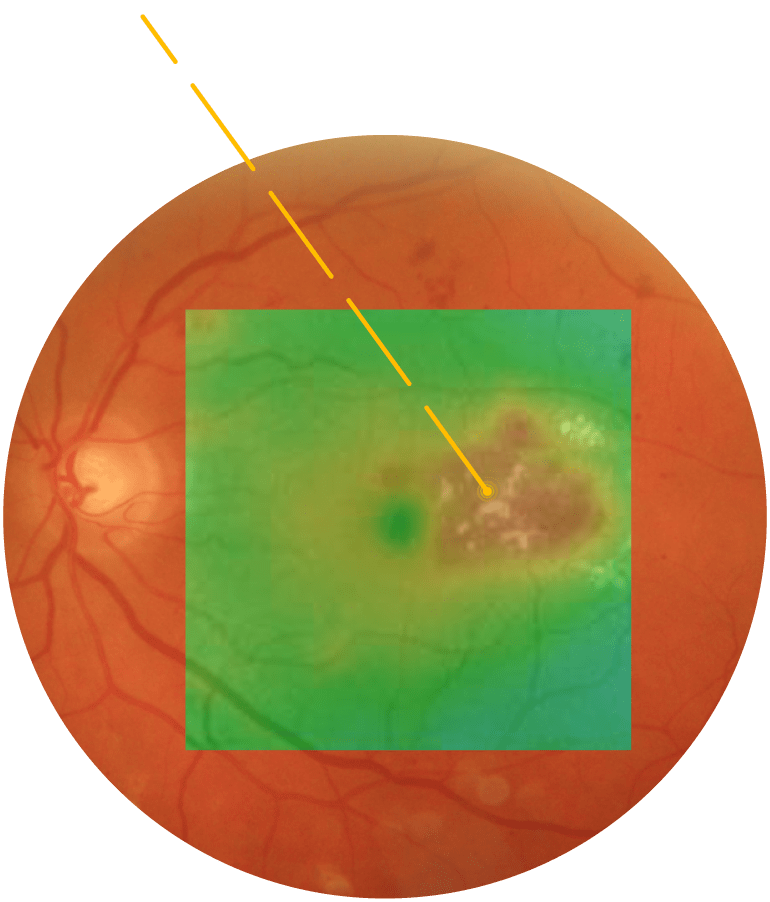
Coriorretinopatía Serosa Central
La coriorretinopatía serosa central (CSC) es una de las causas retinianas más comunes de pérdida de visión. Se caracteriza por un desprendimiento seroso de la retina neurosensorial secundario a una o más lesiones focales del epitelio pigmentario de la retina (EPR)1. Esta patología se encuentra entre las retinopatías más comunes que amenazan la visión, después de DMAE, retinopatía diabética y oclusión de rama venosa retiniana2.
En la CSC aguda, el desprendimiento es causado por una fuga focal en el EPR. Por lo general, se resuelve espontáneamente en unas pocas semanas3. Sin embargo, la CSC crónica puede provocar daños estructurales permanentes y, a menudo, una pérdida pronunciada de la visión central4 5 6.
Hay diferentes opciones de tratamiento disponibles, pero no existe un tratamiento «estándar de oro» para la CSC7crónica :
- La fotocoagulación térmica tradicional se puede utilizar para fugas extrafoveales, pero es destructiva y puede provocar escotomas sintomáticos y neovascularización coroidea.
- Sin embargo, también se puede usar la terapia con láser PDT, incluso cuando se usan entornos de tratamiento reducidos; también hay varios efectos secundarios, como atrofia EPR, neovascularización coroidea, isquemia coriocapillaris y reducción transitoria de la función macular.
- La terapia con láser SubLiminal® amarillo de 577 nm parece ser una estrategia de tratamiento alternativa prometedora8.
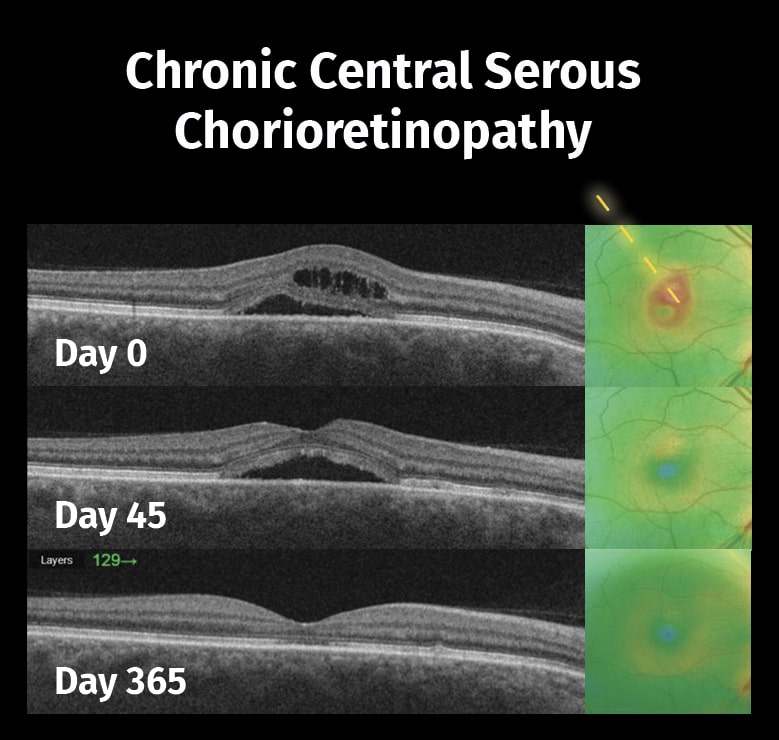
Imágenes: cortesía de Alejandro Filloy Rius, MD. PhD,
Tarragona, España.
Laser for retina
Subthreshold laser therapy guidelines for retinal diseases
Coriorretinopatía Serosa Central sin Visudyne. ¿Es posible?
Central Serous Chorioretinopathy: Can it be treated without Visudyne?
Laser Remains an Effective Option for DME and CSCR Treatments
SubLiminal Laser Therapy for CSC
Safe and Effective Laser Therapies: Targeting Retinal Diseases Amidst COVID-19
The Role of the New Generation of Lasers in Retina
Efficacy and safety of subthreshold micropulse laser compared with threshold conventional laser in CSC
What is the role of Easyret subthreshold laser in macular diseases?
¿Como optimizar el tratamiento láserde la retina en el 2022?
SubLiminal laser for DME and CSC: when and how?
SubLiminal laser for cCSC management
Yellow subthreshold laser vs pdt in eyes with CCSC
Subliminal laser for the treatment of Central Serous Chorioretinopathy
Our first year of lessons learnt with SubLiminal laser for CCSC and DME
Edema macular diabético
La retinopatía diabética es la principal causa de pérdida visual y ceguera en las poblaciones en edad de trabajar en el mundo desarrollado. El edema macular diabético (EMD) es la principal causa de ceguera en la población diabética.
Un análisis conjunto reciente de 35 estudios poblacionales estimó que 93 millones de personas en todo el mundo tienen retinopatía diabética, de las cuales 17 millones (un 18%) tienen RD proliferativa, 21 millones (un 23%) tienen edema macular diabético (EMD) y 28 millones (un 20%) tienen DR9 que amenaza la vista.
El tratamiento del EMD ha cambiado significativamente en los últimos años. Sin embargo, la mejor opción de tratamiento aplicable a todos los pacientes con EMD sigue siendo una cuestión abierta. Aunque la introducción de terapias anti-VEGF ha demostrado su seguridad y eficacia, el láser aún juega un papel importante1011
La terapia con láser amarillo de 577 nm SubLiminal® puede ser un excelente complemento o alternativa a las terapias anti-VEGF.
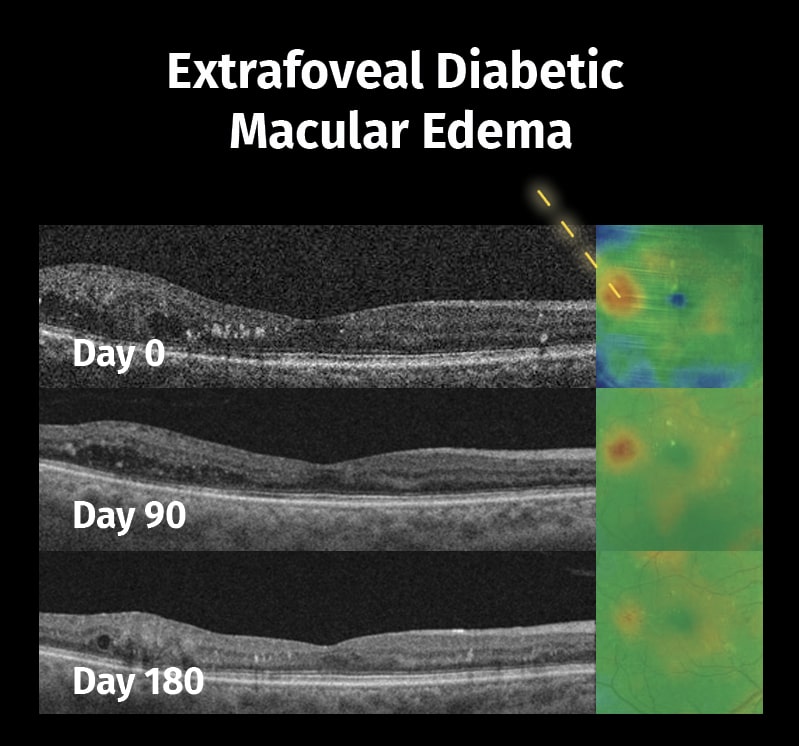
Imágenes: cortesía de Alejandro Filloy Rius, MD. PhD,
Tarragona, España.
Laser for retina
Laser Remains an Effective Option for DME and CSCR Treatments
SubLiminal Laser for Center-Involving Diabetic Macular Edema
An Exciting Journey in SubLiminal Laser Treatment Therapy for DME
Subthreshold yellow laser for fovea-involving diabetic macular edema in a series of patients with good vision
Macular laser photocoagulation in the management of diabetic macular edema: Still relevant in 2020?
Management of cystoid macular edema secondary to retinitis pigmentosa via subliminal micropulse yellow laser
Comparison of ranibizumab and subthreshold micropulse laser in treatment of macular edema secondary to branch retinal vein occlusion
Laser Remains An Effective Treatment Option for DME
What is the role of Easyret subthreshold laser in macular diseases?
¿Como optimizar el tratamiento láserde la retina en el 2022?
SubLiminal Laser for predominantly non-center involving DME?
Transfoveal SubLiminal Laser treatment for CSC
SubLiminal laser for DME and CSC: when and how?
Fovea-Involving DME: Reasons for the subliminal approach
Our first year of lessons learnt with SubLiminal laser for CCSC and DME
Degeneración macular asociada a la edad
La degeneración macular relacionada a la edades la principal causa mundial de ceguera irreversible entre las personas mayores.
La DMAE atrófica (DMAE seca) afecta aproximadamente al 80-90% de las personas con DMAE.
En la DMAE temprana se forman pequeños depósitos blancos o amarillentos (llamados drusas) en la retina, debajo de la mácula, lo que hace que se deteriore o degenere con el tiempo.
Las drusas duras son lesiones pequeñas, bien delimitadas, y pueden verse en la población sana y de la tercera edad.
Las drusas blandas son grandes y sus bordes están menos definidos (como una bola de algodón). Por lo general son patológicas y no se encuentran en poblaciones jóvenes y sanas.
Actualmente no existe un tratamiento para las drusas; sin embargo, se ha observado clínicamente que el láser subumbral podría hacerlas desaparecer y prevenir la progresión de la patología.
Actualmente se están realizando estudios clínicos sobre este tema.
Vasculopatía coroidea polipoide idiopática (IPCV)
La vasculopatía coroidea polipoidea idiopática (IPCV)es una enfermedad de la vasculatura coroidea.
Se caracteriza por la presencia de lesiones polipoideas aneurismáticas y una red vascular ramificada en la vasculatura coroidea. Esto puede provocar el desprendimiento del epitelio pigmentario (DEP) seroso o hemorrágico, episodios de desprendimiento de retina exudativo y exudación y hemorragia subretiniana.
Se considera una variante de la DMAE neovascular.
La IPCV es relativamente común en las poblaciones asiática y afroamericana y afecta a ambos sexos.
La evidencia sostiene que:
- Los pacientes sintomáticos de IPCV pueden tener una regresión completa sin pérdida severa de la visión a partir de terapia fotodinámica (TFD) y tratamiento anti-VEGF.
- El láser SubLiminal de 577 nm se puede utilizar para complementar el tratamiento en casos de IPCV con una respuesta subóptima al tratamiento anti-VEGF.
Efficacy of SubLiminal laser in IPCV Aflibercept resistant cases
Physicians
Talk about SubliminalLaser Therapy




Bibliografía
Central serous chorioretinopathy (CSCR) is a common retinal cause of vision loss. This review surveys the epidemiology, risk factors, clinical presentation, natural history and pathophysiology of CSCR. Studies suggest an annual incidence rate of 10 per 100 000 in men, with CSCR occurring six times more commonly in men compared with women. Most acute CSCR cases resolve spontaneously within 2–3 months. Prognosis is highly dependent on presenting visual acuity; patients with initial visual acuities of 6/6 remain at that level, while patients with initial visual acuities of less than 6/9 recover on average two to three Snellen lines over the next few years. The main risk factors for CSCR are systemic corticosteroid use, type A personality, pregnancy and endogenous Cushing’s syndrome. The pathophysiology of CSCR remains obscure, although disorders in both the choroidal circulation and retinal pigment epithelium are implicated.
Central serous chorioretinopathy (CSC) is a disease of the retina characterized by serous detachment of the neurosensory retina secondary to one or more focal lesions of the retinal pigment epithelium (RPE). CSC occurs most frequently in mid-life and more often in men than in women. Major symptoms are blurred vision, usually in one eye only and perceived typically by the patient as a dark spot in the centre of the visual field with associated micropsia and metamorphopsia. Normal vision often recurs spontaneously within a few months. The condition can be precipitated by psychosocial stress and hypercortisolism. Ophthalmoscopic signs of CSC range from mono- or paucifocal RPE lesions with prominent elevation of the neurosensory retina by clear fluid – typical of cases of recent onset – to shallow detachments overlying large patches of irregularly depigmented RPE.
Data are presented from 27 patients (34 eyes) with central serous choroidopathy who were followed up for an average of 23 months without therapeutic intervention. The detachment completely resolved in all cases. The average duration of detachment was three months. In all eyes, the visual acuity returned to 20/40 or better, and in all but two eyes, the final visual acuity was 20/30 or better. Central serous choroidopathy is essentially a benign and self-limited disorder, and treatment by photocoagulation is seldom needed.
The Wilmer Retinal Vascular Center’s experience with central serous chorioretinopathy from 1970 to the end of 1979 was reviewed and compared with previous studies. Retrospective analysis of 73 patients seen at follow-up suggests no clinically significant effect of focal argon laser photocoagulation on final visual acuity or recurrence rate. Patients with initial visual acuity of 20/20 remained at that level, and patients with initial visual acuity of less than 20/30 gained, on average, two to three Snellen lines at follow-up. Approximately one-third of both untreated and treated patients had recurrence or presumed persistence during the follow-up period. With the inclusion of episodes that occurred before the first Wilmer Institute visit about half of each group had recurrence or presumed persistence. Recurrences were most often due to leakage from a site within one disc diameter of the original site of leakage.
In a prospective randomised trial of argon laser photocoagulation in the management of central serous retinopathy, long-term follow-up (6.4 to 12.1 years) revealed no evidence that treatment significantly influenced the visual outcome as measured by the Snellen chart and by the Farnsworth-Munsell 100-hue test. Treatment did not reduce either the recurrence rate or the prevalence of chronic disease. Complications of treatment were uncommon. The justification for argon laser photocoagulation appears to be limited to the hastening of symptomatic relief by earlier resolution of serous detachment.
Background: To evaluate risk factors for the recurrence of serous macular detachment in untreated patients with central serous chorioretinopathy (CSC).
Methods: Retrospective review of untreated CSC patients with a follow-up of ≥3 years. Patient demographics, visual outcome and risk factors for the recurrence of CSC were analyzed.
Results: Seventy-three eyes of 73 patients were included, and the mean age was 44.6 years. At baseline, the mean logMAR best corrected visual acuity (BCVA) was 0.30. After a mean follow-up of 72 months, the mean final logMAR BCVA was 0.32. The difference between the final and baseline BCVAs was not statistically significant (p = 0.79). At the last follow-up, 9 (12.3%) eyes showed improved vision of ≥2 lines, and 12 (16.4%) showed a worsening of ≥2 lines. During follow-up, 38 (52.1%) patients experienced ≥1 episode of CSC recurrence. Multivariate Cox regression analysis showed that patients with a history of psychiatric illness (adjustment disorder and depression) were associated with an increased risk of CSC recurrence (hazard ratio = 3.5, p = 0.011).
Conclusions: The long-term visual prognosis of CSC is fair without treatment, and a significant proportion of patients developed recurrence of CSC. A history of psychiatric illness is associated with an increased risk of CSC recurrence.
Purpose: To assess treatment with a 577-nm subthreshold micropulse laser (SML) in patients with chronic central serous chorioretinopathy (cCSC).
Methods: This retrospective study included 38 patients treated with a 577-nm SML (Supra Scan; Quantel Medical) for cCSC. We included a subgroup of 18 patients with persistent subretinal fluid (SRF) after photodynamic therapy (PDT). Assessment included visual acuity (VA), central retinal thickness (CRT) and resolution of SRF.
Results: At the last follow-up (mean 5 months), 74% of patients responded to therapy. The CRT decreased after treatment (mean CRT -115 µm, p < 0.001) and VA improved (mean logMAR -0.06, p = 0.039). No laser burns were detected with any imaging modality. In the subgroup of patients resistant to PDT, 61% of patients responded to therapy with a decrease in CRT (mean CRT -75 µm, p = 0.019).
Conclusions: The 577-nm SML is an effective treatment for cCSC even in patients without sufficient improvement after PDT.
Purpose: To compare the short-term treatment outcome of the 577 nm subthreshold micropulse laser (SML) and half-dose photodynamic therapy (PDT) in patients with chronic central serous chorioretinopathy (cCSC) and persistent subretinal fluid (SRF).
Methods: This retrospective study included 100 eyes of 100 consecutive patients who were treated with the 577 nm SML (Supra Scan, Quantel Medical) (n=42) or half-dose PDT (n=58) for cCSC. The treatment was applied at the leakage sites in the fluorescein and indocyanine green angiography. The treatment success was evaluated 6 weeks after treatment using best-corrected visual acuity, central retinal thickness, and resolution of SRF in spectral domain optical coherence tomography.
Results: Patients showed treatment response more often in the SML group compared with the PDT group (treatment response after SML: 33 eyes (79%), PDT: 34 eyes (59%), P=0.036, χ2 test). The CRT decreased significantly after both treatments (mean CRT before SML: 445±153 μm, after SML: 297±95, Po0.001; mean CRT before PDT: 398±88 μm, after PDT: 322±93 μm, Po0.001, Wilcoxon’s signed-rank test). The decrease in CRT was statistically significantly higher in the SML group (decrease in CRT after SML: − 148±163 μm, after PDT: −76±104 μm, P=0.041, Mann–Whitney U-test).
Conclusions: Both the half-dose PDT and the 577 nm SML are potent treatments for cCSC with persistent SRF. More patients showed treatment response to the SML treatment and SML leads to a greater decrease in CRT.
Objective: To examine the global prevalence and major risk factors for diabetic retinopathy (DR) and vision-threatening diabetic retinopathy (VTDR) among people with diabetes.
Research design and methods: A pooled analysis using individual participant data from population-based studies around the world was performed. A systematic literature review was conducted to identify all population-based studies in general populations or individuals with diabetes who had ascertained DR from retinal photographs. Studies provided data for DR end points, including any DR, proliferative DR, diabetic macular edema, and VTDR, and also major systemic risk factors. Pooled prevalence estimates were directly age-standardized to the 2010 World Diabetes Population aged 20-79 years.
Results: A total of 35 studies (1980-2008) provided data from 22,896 individuals with diabetes. The overall prevalence was 34.6% (95% CI 34.5-34.8) for any DR, 6.96% (6.87-7.04) for proliferative DR, 6.81% (6.74-6.89) for diabetic macular edema, and 10.2% (10.1-10.3) for VTDR. All DR prevalence end points increased with diabetes duration, hemoglobin A(1c), and blood pressure levels and were higher in people with type 1 compared with type 2 diabetes.
Conclusions: There are approximately 93 million people with DR, 17 million with proliferative DR, 21 million with diabetic macular edema, and 28 million with VTDR worldwide. Longer diabetes duration and poorer glycemic and blood pressure control are strongly associated with DR. These data highlight the substantial worldwide public health burden of DR and the importance of modifiable risk factors in its occurrence. This study is limited by data pooled from studies at different time points, with different methodologies and population characteristics.
Subthreshold, or tissue-sparing, laser therapy is a subject of interest to retinal specialists worldwide. Today, micropulse technology with 810 nm and 577 nm lasers is used to produce a therapeutic treatment without inducing intraretinal damage detectable on clinical examination during or after treatment. The controlled laser delivery of micropulse technology affords treatment options for diabetic macular edema(DME), proliferative diabetic retinopathy (PDR), central erous chorio retinopathy (CSR), macular edema secondary to branch retinal vein occlusion (BRVO), and even glaucoma. This review will explain micropulse technology and focus on its benefits and challenges in the treatment of retinal disorders.
Purpose: This pilot study aimed to evaluate the efficacy and safety of subthreshold micropulse yellow (577-nm) laser photocoagulation (SMYLP) in the treatment of diabetic macular edema (DME).
Methods: We reviewed 14 eyes of 12 patients with DME who underwent SMYLP with a 15% duty cycle at an energy level immediately below that of the test burn. The laser exposure time was 20 ms and the spot diameter was 100 µm. Laser pulses were administered in a confluent, repetitive manner with a 3 × 3 pattern mode.
Results: The mean follow-up time was 7.9 ± 1.6 months. The baseline-corrected visual acuity was 0.51 ± 0.42 logarithm of the minimum angle of resolution (logMAR), which was improved to 0.40 ± 0.35 logMAR (p = 0.025) at the final follow-up. The central macular thickness at baseline was 385.0 ± 111.0 µm; this value changed to 327.0 ± 87.7 µm (p = 0.055) at the final follow-up.
Conclusions: SMYLP showed short-term efficacy in the treatment of DME and did not result in retinal damage. However, prospective, comparative studies are needed to better evaluate the efficacy and safety of this treatment.
Keywords: Diabetic retinopathy; Laser therapy; Macular edema.